Surgical Techniques to Prevent Osteoarthritis
Knee Joint Preservation Techniques
The information below is generalized. Patients’ treatments can vary depending on injury size and any concomitant procedures done.
MACI (Matrix-induced Autologous Chondrocyte Implantation)
- Two-part procedure commonly used to treat cartilage defects/lesions of the knee or kneecap
- Patient’s own cells are harvested, grown, and reimplanted
- 1st Arthroscopic Procedure – Cartilage biopsy/harvest
- Evaluation of the condition of the cartilage, remove damaged tissue from the knee (if necessary), and harvest a bit of cartilage from non-weightbearing regions of the knee
- Procedure takes ~30 minutes and involves 2 small incisions
- Following the first procedure, the patient can immediately bear weight and return to activity as tolerated. Most can return to work within a day or two.
- Cartilage Preparation
- Harvested cartilage is sent to a laboratory to grow on a collagen membrane/matrix for approximately one month
- New cartilage cells are stored and usable for up to 5-years.
- Harvested cartilage is sent to a laboratory to grow on a collagen membrane/matrix for approximately one month
- 2nd Open Procedure – Cartilage Implantation
- Newly grown cartilage is cut to precisely fit the patient’s defect and glued into place
- Procedure takes ~1 hour and involves an open approach with a larger incision
- Following the second procedure, patients will be expected to wear a brace for 6 weeks and use a continuous passive motion machine (CPM). Patients will start physical therapy 4-6 weeks after surgery. However, recovery timelines may differ if additional procedures are needed.
- Your specific recovery timeline will be clearly outlined by Dr. Martin at the time of the procedure.
Osteochondral Grafting
- Commonly used to treat lesions/defects in the knee that involve both cartilage and underlying bone
- Replaces lesion with healthy tissue (the graft)
- Depending on the size of the lesions, the graft my come from
- Patient’s own body (osteochondral autograft)
- If lesion is small (< 2cm), the graft can come from peripheral non-weight bearing areas of the patients knee
- Tissue donor (osteochondral allograft)
- If the lesion is medium or large (> 2cm), the graft will come from a tissue donor
- Patient’s own body (osteochondral autograft)
- Joint malalignment, ligamentous instability, and meniscal deficiency may be addressed at the time of surgery (if indicated)
- Maximizes longevity of the graft and prevents additional damage or injury
- Following surgery, patients will be expected to wear a brace, refrain from weight bearing, and use a continuous passive motion machine (CPM) for 6 weeks. After 6 weeks, patients can gradually increase weight bearing and forgo the use of a brace. Return to sport typically occurs after 6-9 months.
- Your specific recovery timeline will be clearly outlined by Dr. Martin at the time of the procedure.
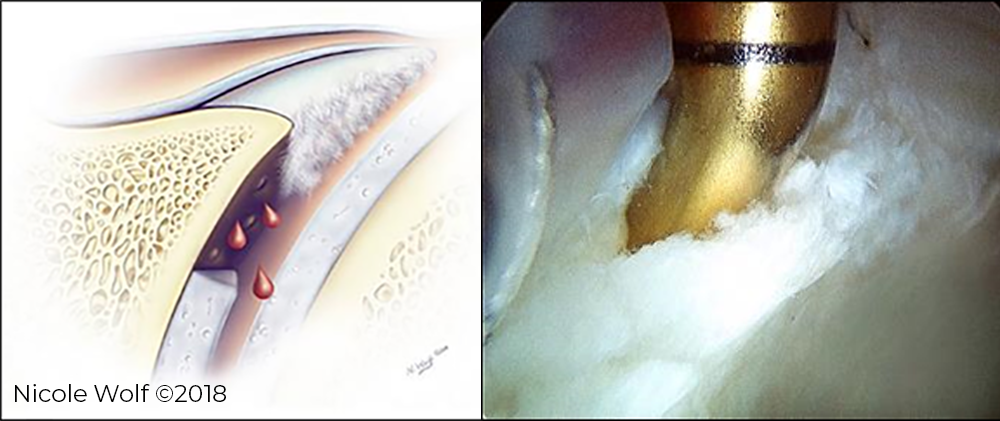
Microfracture
- Commonly used to treat cartilage lesions/defects that expose the underlying bone in the knee by using the body’s own healing abilities
- Performed arthroscopically through three small incisions
- First, the surgeon evaluates the lesion and removes any loose or unstable cartilage, ensuring a smooth and stable cartilage surface surrounds the lesion.
- Multiple holes, or ‘microfractures’, are then created in the bone underneath the lesion.
- Blood and bone marrow cells travel through the holes and combine on the surface of the lesion, forming a “marrow-rich clot” that serves as the basis for new tissue formation.
- New tissue formation is a gradual process
- It may take 2-6 months after surgery for patients to experience significant improvement in pain and function
- Following surgery, patients will be expected to wear a brace, refrain from weight bearing, and use a continuous passive motion machine (CPM) for 6 weeks. After 6 weeks, patients can gradually increase weight bearing and forgo the use of a brace. Return to sport typically occurs after 6-9 months.
- Your specific recovery timeline will be clearly outlined by Dr. Martin at the time of the procedure.