These findings highlight the importance of analyzing spinopelvic parameters preoperatively to prognosticate outcomes before hip arthroscopy for acetabular labral tears and FAI.
Torabian KA, Cherian NJ, Eberlin CT, Dean MC, Dowley KS, LaPorte ZL, Kucharik MP, Gillinov SM, Martin, SD. High Pelvic Incidence Predicts Inferior Outcomes Following Hip Arthroscopy for Femoroacetabular Impingement and Acetabular Labral Tears. Am J Sports Med. 2024 Mar;52(3):631-642. https://doi.org/10.1177/03635465231219261 PMID: 38369972 PMCID: PMC10905981
Abstract
Background
In the setting of femoroacetabular impingement (FAI), decompression osteoplasties reconcile deleterious loading patterns caused by cam and pincer lesions. However, native variations of spinopelvic sagittal alignment may continue to perpetuate detrimental effects on the labrum, chondrolabral junction, and articular cartilage after hip arthroscopy.
Purpose
To evaluate the effect of pelvic incidence (PI) on postoperative outcomes after hip arthroscopy for acetabular labral tears in the setting of FAI.
Methods
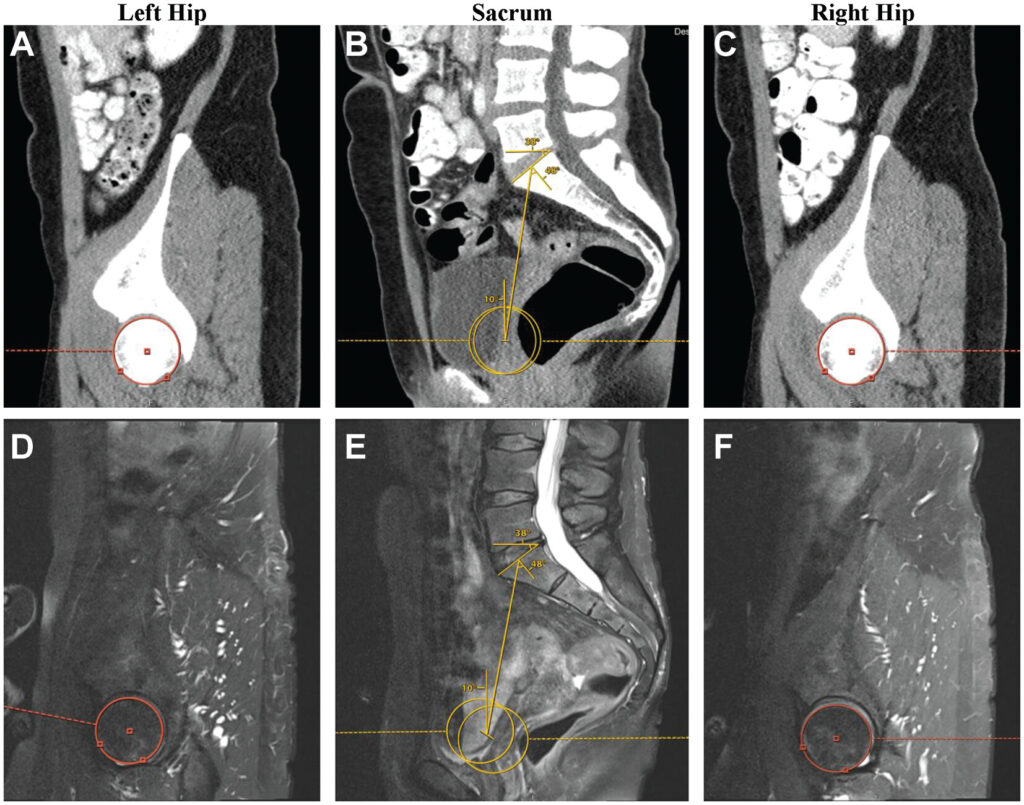
A retrospective query of prospectively collected data identified patients ≥18 years of age who underwent primary hip arthroscopy for FAI and acetabular labral tears between February 2014 and January 2022, with 3-, 6-, 12-, and 24-month follow-ups. Measurements for PI, pelvic tilt (PT), sacral slope (SS), and acetabular version were obtained via advanced diagnostic imaging. Patients were stratified into low-PI (<45°), moderate-PI (45°≤ PI ≤ 60°), and high-PI (>60°) cohorts. Patient-reported outcome measures (PROMs), clinically meaningful outcomes (ie, minimal clinically important difference, Patient Acceptable Symptom State, substantial clinical benefit, and maximal outcome improvement), visual analog scale (VAS) pain scores, and patient satisfaction were compared across cohorts.
Results
A total of 74 patients met eligibility criteria and were stratified into low-PI (n = 28), moderate-PI (n = 31), and high-PI (n = 15) cohorts. Correspondingly, patients with high PI displayed significantly greater values for PT (P = .001), SS (P < .001), acetabular version (P < .001), and acetabular inclination (P = .049). By the 12- and 24-month follow-ups, the high-PI cohort was found to have significantly inferior PROMs, VAS pain scores, rates of clinically meaningful outcome achievement, and satisfaction relative to patients with moderate and/or low PI. No significant differences were found between cohorts regarding rates of revision arthroscopy, subsequent spine surgery, or conversion to total hip arthroplasty.
Conclusion
After hip arthroscopy, patients with a high PI (>60°) exhibited inferior PROMs, rates of achieving clinically meaningful thresholds, and satisfaction at 12 and 24 months relative to patients with low or moderate PI. Conversely, the outcomes of patients with low PI (<45°) were found to match the trajectory of those with a neutral spinopelvic alignment (45°≤ PI ≤ 60°). These findings highlight the importance of analyzing spinopelvic parameters preoperatively to prognosticate outcomes before hip arthroscopy for acetabular labral tears and FAI.